#diabeteshomeopathy #diabeteshomeopathyclinic #diabeteshomeopathytreatment #diabeteshomeopathydoctorinchennai #diabeteshomeopathicclinicinchennai #diabeteshomeopathictreatmentinchennai
Diabetes, a chronic condition affecting millions worldwide, is more than just a diagnosis; it's a lifestyle. With its prevalence on the rise globally, understanding diabetes and how to manage it effectively is crucial for both individuals living with the condition and those around them. In this comprehensive guide, we'll delve into what diabetes is, its types, symptoms, risk factors, management strategies, and the importance of education and support in navigating this journey towards better health.
What is Diabetes?
Diabetes mellitus, commonly referred to as diabetes, is a metabolic disorder characterized by high blood sugar levels over a prolonged period. This elevation in blood glucose levels occurs either due to inadequate production of insulin (a hormone produced by the pancreas that regulates blood sugar) or the body's inability to effectively use the insulin it produces. As a result, glucose remains in the bloodstream, leading to various complications if left uncontrolled.
Diabetes is a chronic metabolic disorder characterized by high levels of glucose (sugar) in the blood. There are several types of diabetes, each with its own causes, risk factors, and management strategies:
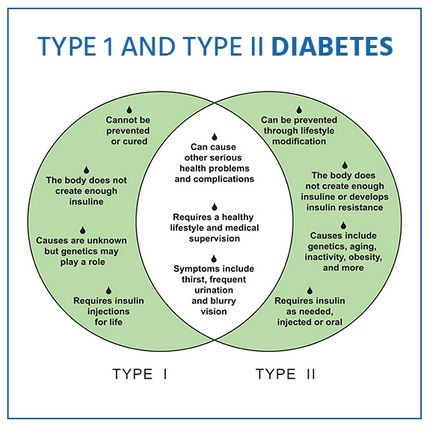
Type 1 Diabetes: Type 1 diabetes, formerly known as juvenile diabetes or insulin-dependent diabetes, is an autoimmune condition in which the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the pancreas produces little to no insulin. People with type 1 diabetes require lifelong insulin therapy to survive. Type 1 diabetes usually develops in childhood or adolescence, but it can occur at any age.
Type 2 Diabetes: Type 2 diabetes is the most common form of diabetes, accounting for the majority of cases. It typically develops in adults, although it is increasingly being diagnosed in children and adolescents due to rising rates of obesity and sedentary lifestyles. In type 2 diabetes, the body becomes resistant to the effects of insulin, and the pancreas may not produce enough insulin to compensate. This leads to elevated blood sugar levels. Type 2 diabetes is often associated with lifestyle factors such as obesity, physical inactivity, and poor diet. It may be managed with lifestyle modifications, oral medications, injectable medications, and/or insulin therapy.
Gestational Diabetes: Gestational diabetes mellitus (GDM) occurs during pregnancy and is characterized by elevated blood sugar levels that develop or are first recognized during pregnancy. It usually resolves after childbirth, but women who have had gestational diabetes have an increased risk of developing type 2 diabetes later in life. Gestational diabetes can increase the risk of complications for both the mother and the baby during pregnancy and delivery. Management typically involves dietary changes, monitoring blood sugar levels, and, in some cases, insulin therapy.
Monogenic Diabetes: Monogenic diabetes is a rare form of diabetes caused by mutations in a single gene. These genetic mutations affect the function of the pancreas and insulin production or processing. Monogenic diabetes can present similarly to either type 1 or type 2 diabetes, but it is caused by specific genetic abnormalities. Treatment may vary depending on the specific genetic mutation involved.
Secondary Diabetes: Secondary diabetes refers to diabetes that develops as a result of another medical condition or factor, such as pancreatic disease, hormonal disorders, certain medications (e.g., corticosteroids), or genetic syndromes. Managing the underlying condition or factor is essential in managing secondary diabetes.
Other Specific Types: This category includes various rare forms of diabetes that don't fit into the aforementioned categories, such as diabetes associated with certain genetic syndromes, diseases of the pancreas, or drug-induced diabetes.
Causes of Diabetes
The causes of diabetes vary depending on the type of diabetes:
Type 1 Diabetes:
Autoimmune Destruction: Type 1 diabetes is primarily an autoimmune condition, where the body's immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. The exact cause of this autoimmune response is not fully understood, but it likely involves a combination of genetic predisposition and environmental triggers, such as viral infections or certain dietary factors.
Type 2 Diabetes:
Insulin Resistance: In type 2 diabetes, the body becomes resistant to the effects of insulin, and the pancreas may not produce enough insulin to compensate for this resistance. The exact causes of insulin resistance are complex and multifactorial, but they often involve a combination of genetic predisposition and lifestyle factors, such as obesity, physical inactivity, and poor diet. Excess body fat, especially abdominal fat, can contribute to insulin resistance.
Genetic Factors: Genetics plays a significant role in the development of type 2 diabetes. Family history and certain genetic traits can increase the risk of developing the condition. However, genetic predisposition alone is not sufficient to cause type 2 diabetes, and environmental factors also play a crucial role.
Gestational Diabetes:
Hormonal Changes: During pregnancy, the placenta produces hormones that can interfere with the action of insulin, leading to a condition called insulin resistance. This can result in elevated blood sugar levels, especially in women with preexisting insulin resistance or insufficient insulin production. Gestational diabetes typically develops later in pregnancy, around the 24th to 28th week, and usually resolves after childbirth.
Other Types:
Monogenic Diabetes: Monogenic diabetes is caused by mutations in a single gene that affects insulin production or processing. These genetic mutations can be inherited and are responsible for a small percentage of diabetes cases.
Secondary Diabetes: Secondary diabetes refers to diabetes that develops as a result of another medical condition or factor, such as pancreatic disease, hormonal disorders, certain medications (e.g., corticosteroids), or genetic syndromes.
Overall, while genetics plays a significant role in diabetes, lifestyle factors such as diet, physical activity, and body weight also play critical roles, particularly in the development of type 2 diabetes. Preventive measures, such as maintaining a healthy lifestyle and managing risk factors, can help reduce the risk of developing diabetes.
Symptoms of Diabetes:
The symptoms of diabetes can vary depending on the type of diabetes and the individual's health status. Here are common symptoms associated with diabetes:
Frequent Urination (Polyuria): Increased urination is often one of the first signs of diabetes. Excess sugar in the blood leads to increased urine production as the kidneys work to eliminate the excess glucose from the body.
Excessive Thirst (Polydipsia): Increased urination can lead to dehydration, causing excessive thirst. People with diabetes may find themselves drinking more fluids than usual to quench their thirst.
Unexplained Weight Loss: Despite increased appetite and food intake, individuals with diabetes may experience unexplained weight loss. This is often seen in type 1 diabetes, where the body's inability to use glucose for energy leads to the breakdown of fat and muscle tissue.
Fatigue: Feeling unusually tired or lethargic is a common symptom of diabetes. The body's inability to properly utilize glucose for energy can lead to feelings of fatigue and weakness.
Increased Hunger (Polyphagia): Despite eating regularly, individuals with diabetes may feel hungry more often. This is due to the body's inability to properly regulate blood sugar levels, leading to fluctuations in energy levels.
Blurred Vision: High levels of glucose in the blood can cause fluid to be pulled from the lenses of the eyes, affecting their ability to focus properly. This can result in blurred vision and difficulty seeing clearly.
Slow Healing of Wounds: High blood sugar levels can damage blood vessels and nerves, leading to poor circulation and reduced sensation, which can delay the healing process.
Frequent Infections: Individuals with diabetes may be more prone to infections, particularly in the skin, gums, urinary tract, and genital areas.
Numbness or Tingling in Extremities (Neuropathy): Diabetes can damage the nerves, leading to numbness, tingling, or burning sensations, particularly in the hands and feet. This condition, known as neuropathy, can also cause pain and weakness in affected areas.
Other Symptoms: Other symptoms of diabetes may include dry mouth, itchy skin, yeast infections (particularly in women), and erectile dysfunction (in men).
It's important to note that not everyone with diabetes will experience all of these symptoms, and some individuals may not experience any symptoms at all, especially in the early stages of the disease. If you experience any of these symptoms, particularly if they persist or worsen over time, it's important to consult a healthcare professional for proper evaluation and diagnosis. Early detection and treatment of diabetes are crucial for preventing complications and managing the condition effectively.
Risk Factors:
While the exact cause of diabetes isn't fully understood, several factors can increase one's risk of developing the condition, including:
Family history of diabetes
Obesity or being overweight
Sedentary lifestyle
Unhealthy diet high in sugar and processed foods
Age (risk increases with age)
Ethnicity (some ethnic groups are at higher risk)
Complications of Diabetes
Diabetes can lead to various complications if not properly managed. These complications can affect different parts of the body and can be acute or chronic. Here are some common complications associated with diabetes:
Cardiovascular Complications:
Heart Disease: Diabetes significantly increases the risk of developing cardiovascular diseases such as coronary artery disease, heart attack, and stroke.
High Blood Pressure (Hypertension): High blood pressure, which further raises the risk of heart disease and stroke. Neuropathy:
Peripheral Neuropathy: Diabetes can damage the nerves, particularly in the legs and feet, leading to peripheral neuropathy.
Autonomic Neuropathy: Damage to the nerves that control involuntary body functions can lead to problems with digestion, bowel and bladder function, sexual function, and regulation of blood pressure and heart rate. Nephropathy:
Diabetic Nephropathy: Diabetes is a leading cause of kidney disease (nephropathy) leading to decreased kidney function and eventual kidney failure.
Increased Risk of Kidney Stones and Urinary Tract Infections: Diabetes increases the risk of developing kidney stones and urinary tract infections. Eye Complications:
Diabetic Retinopathy: Diabetes can damage the blood vessels in the retina, leading to diabetic retinopathy. This condition can cause vision problems, including blurred vision, floaters, and, in severe cases, vision loss.
Cataracts and Glaucoma: Diabetes also increases the risk of developing cataracts and glaucoma. Foot Complications:
Foot Ulcers and Infections: Diabetes can lead to poor circulation and nerve damage in the feet, increasing the risk of foot ulcers and infections. Poor wound healing and reduced sensation can make these ulcers difficult to treat and prone to complications, including amputation.
Skin Complications:
Skin Infections: Diabetes can increase the risk of various skin infections, including bacterial and fungal infections.
Dry Skin and Itching: Diabetes can cause dry, itchy skin due to changes in skin moisture levels and impaired nerve function.
Mental Health Complications:
Depression and Anxiety: Diabetes is associated with an increased risk of depression and anxiety, possibly due to the stress of managing the condition, hormonal changes, and biochemical imbalances.
Cognitive Decline: Some studies suggest that diabetes may be a risk factor for cognitive decline and dementia, although the exact mechanisms are not fully understood.
Diabetes homeopathy treatment in Chennai.
Frequently Asked Questions
Q: What should my blood sugar be when I wake up (fasting) and before meals? What about after?
A: For most people with diabetes, the American Diabetes Association recommends a fasting or before-meals blood glucose (or blood sugar) goal of 70–130 mg/dl. One to two hours after eating, a postprandial blood sugar reading at or under 180 mg/dl is recommended.
Q: Will insulin make me gain weight?
A: The reason we need insulin-as a hormone made in our bodies or as a medication-is to push glucose into cells for energy. Insulin's job is to process calories. For this reason, it can-but doesn't have to-cause weight gain.
Q: Is it true that complications of diabetes can be delayed and even prevented?
A: Yes! Diabetes when diagnosed and the sooner you start to aggressively get your blood sugar, blood pressure, and cholesterol into target ranges, the healthier you can be over the years. To stay healthy and detect any complications early, make sure your health care provider orders all the tests and checks you need.
Q: Are my children at risk?
A: Yes. Type 2 diabetes is a genetic disease. The risk is highest when multiple family members have diabetes, and if the children also are overweight, sedentary and have the other risk factors for type 2 diabetes. Your child has a 10-15% chance of developing type 2 diabetes when you have type 2 diabetes. And if one identical twin has type 2 diabetes, there is a 75% likelihood of the other twin developing type 2 diabetes also.
Q: Do I need to monitor my blood sugar when I have type 2 diabetes?
A: You may feel fine, but that is no guarantee that your blood sugar levels are in the target range. Remember, diabetic complications do not appear right away. And complications may develop even when the blood sugar is only slightly elevated. Regular blood sugar monitoring can help you keep your blood sugars in control and prevent serious damage to your eyes, kidneys and nerves. If your sugar levels are out of line, consult your doctor.